Aim
The aim of this good practice point is to standardise care regarding the measurement of fundal height in pregnancy and the detection of abnormal growth.
Assess risk of FGR
- Risk assessment for FGR should be undertaken as early in pregnancy as possible.
- At first visit, confirm estimated due date (EDD) by comparing last normal menstrual period (LNMP) and early ultrasound (US). If the LNMP was uncertain or menstruation irregular, use the EDD from any US performed between 6 and 24 weeks gestation. If the LNMP was certain and menstruation regular, use the EDD given by LNMP if the dates differ by 5 days or less for early US (between 6 and 13 weeks) or 10 days or less for later US (between 13 and 24 weeks). Use the EDD given by US if the dates differ by 5 days or more for early US (between 6 and 13 weeks) or 10 days or more for later US (between 13 and 24 weeks) (Safer Care Victoria, 2020).
- Where modifiable risk factors for FGR are identified (e.g. smoking), follow recommended care for example, smoking cessation, low dose aspirin (LDA) if assessed as high risk of pre-eclampsia.
- Document level of risk using available risk assessment tools (Stillbirth CRE, 2023).
- Risk should be reviewed at each visit.
Measuring fundal height
- All staff should use a standardised technique for fundal height measurement. Bed heads should be set at the same incline and the bladder should be empty.
- A non-elastic tape should be used to measure from the top of the fundus to the top of the symphysis pubis. The tape markings should be down in order to reduce bias.
- Symphyseofundal height (SFH) should be performed each visit from 24 weeks gestation at 2-4 weekly intervals.
- The SFH should be recorded for each visit and the chart reviewed.
- Women with large uterine fibroids are unsuitable for SFH measurements and require screening growth US according to the local service protocol.
- Women with a BMI > 40 are unsuitable for SFH measurements and require screening growth US according to the local service protocol.
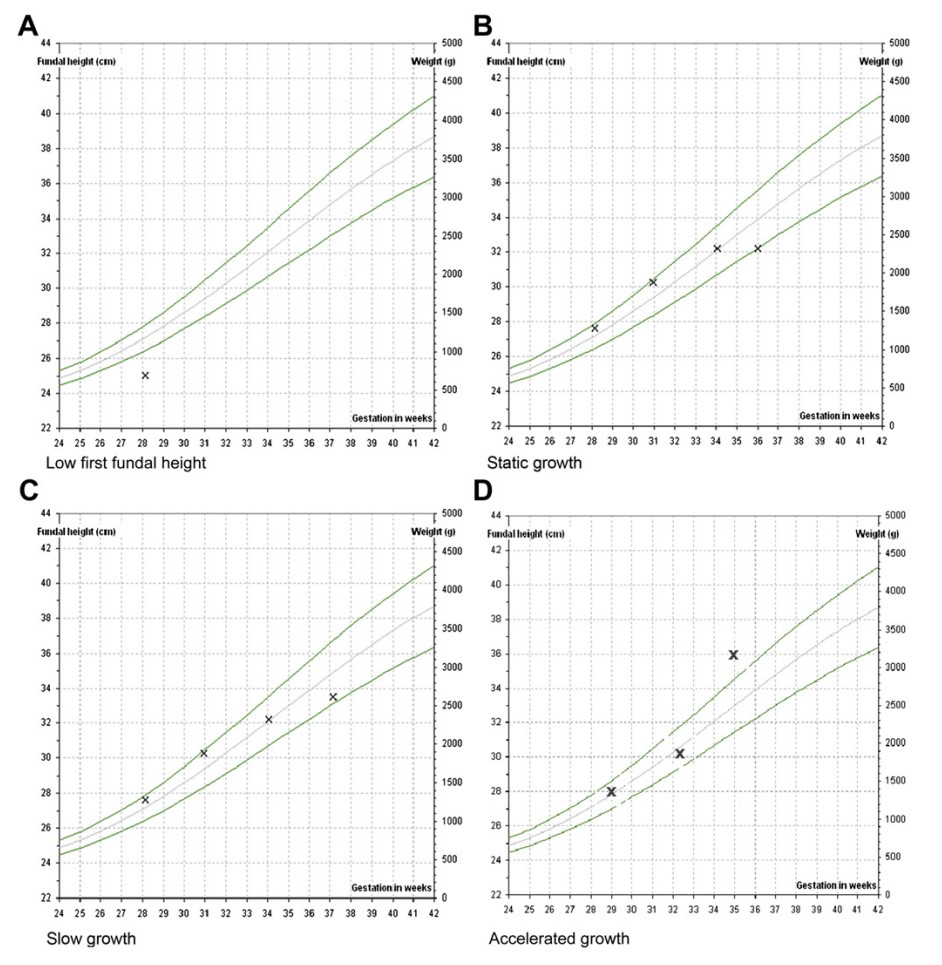
Patterns of abnormal growth
- Where the SFH measures <10th centile at the first measurement, an US is recommended
- Static fundal height (B) and slow growth (C) can be seen in figure 1.
- Management of static fundal height is to refer for US or at term, consider induction of labour.
- Management is to refer for US or at term, consider induction of labour.
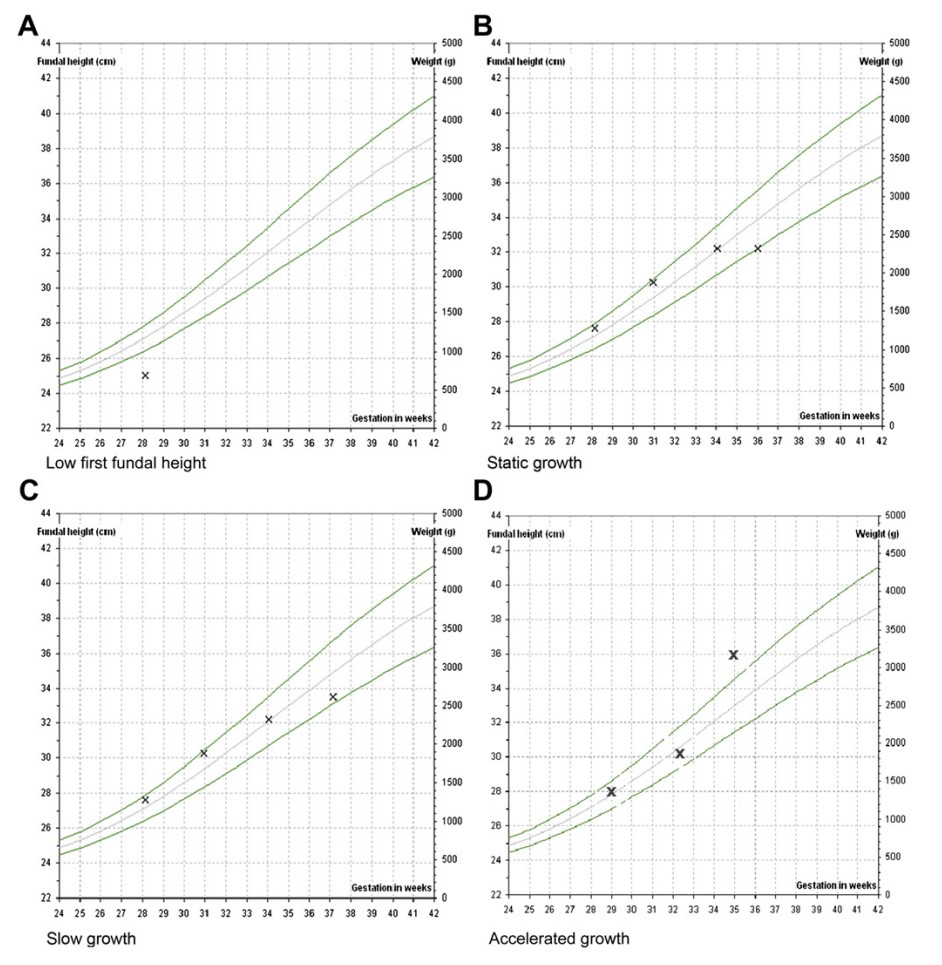
Figure 1. examples of abnormal growth (Morse, Williams and Gardosi, 2009)
Investigations
The following investigations are commonly used for the diagnosis and management of FGR:
- ultrasound assessment of fetal biometry
- amniotic fluid measurement
- umbilical artery Doppler and cardiotocography.
- Additional investigations such as middle cerebral artery doppler, ductus venosus doppler, uterine artery doppler and biophysical profile scoring are individualised according to the clinical circumstances and specialist preference.
References
Morse, K., Williams, A. and Gardosi, J., 2009. Fetal growth screening by fundal height measurement. Best practice & research Clinical obstetrics & gynaecology, 23(6), pp.809-818.
Safer Care Victoria. 2020. Accurate pregnancy dating (estimated due date), Maternity eHandbook. available at: https://www.safercare.vic.gov.au/best-practice-improvement/clinical-guidance/maternity/accurate-pregnancy-dating-estimated-due-date
Stillbirth CRE Position Statement on detection and management of fetal growth restriction in singleton pregnancies available at: https://learn.stillbirthcre.org.au/wp-content/uploads/2023/05/FGR_Position-Statement_V2_August2023.pdf