Acknowledgement
This guidance may use the terms ‘woman’ and ‘mother,’ which are intended to be inclusive of anyone who may use other self-identifying terms and aims to encompass all for whom this guidance is relevant.
Consumer Engagement Statement
All interactions between health care staff with consumers (women, mothers, patients, carers and families) should be undertaken with respect, dignity, empathy, honesty and compassion.
Health care staff should actively seek and support consumer participation and collaboration to empower them as equal partners in their care.
Development of cleft lip and palate
The lip and palate begin forming during just the first few weeks of gestation, often before a woman even knows she is pregnant. During this time, the roof of the mouth begins developing and eventually the two sides of the palate unite evenly in most infants. In some cases, however, the roof of the mouth does not fuse together properly, creating a cleft palate. The cleft may extend through to involve the lip as well. 1
Diagnosis of cleft lip and palate
A cleft lip is often detected on ultrasound at 20 weeks gestation; however a cleft palate can be more difficult to detect at this time. A thorough examination of a baby’s face and mouth at birth is required to diagnose the type and severity of cleft.
Incidence and risk factors for cleft lip and palate
- Cleft lip, cleft palate and cleft lip and palate are among the most common congenital deformities and affect 1.1 in 1000 infants. 2
- Approximately 70% of infants with cleft lip and palate and 50% of infants with cleft palate only are non-syndromic. A small percentage of affected infants may have abnormalities elsewhere in the face or in other parts of their bodies. 3
- The exact cause of cleft lip and palate is unclear; however it is thought that both genetic and environmental factors may contribute. 1
- Some factors that may increase a child’s chance of being born with a cleft lip or palate include; smoking, alcohol consumption or some medications taken during pregnancy. 4
- The chance of developing a cleft increases if other family members are affected.
Cleft lip
A cleft lip is an abnormal gap or opening in the upper lip. Sometimes the upper gum (alveolus) can also be affected. Normally the lip is formed during weeks 4 – 6 of pregnancy. If for some reason the parts of the lip do not come together properly, the baby is born with a cleft lip. 5
Clefts of the lip can present in several ways. A complete cleft of the lip is where the opening extends from the lip all the way up to the nostril. An incomplete cleft lip is where the gap in the lip ends before reaching the nostril, leaving some tissue joined below the nostril. Clefts of the lip can occur on one side of the lip (unilateral) or two sides of the lip (bilateral). 5
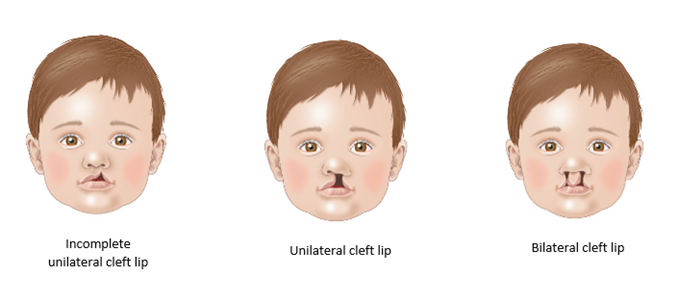
Figure 1. Types of cleft lip
Other conditions associated with cleft lip
Deformity of the nose is frequently associated with a cleft lip. The nose deformity is usually attended to at the time of lip surgery, with great improvement, however further surgery is often needed to improve the appearance of the nose. This is preferably should be done after the face has finished growing in adolescence, although sometimes this surgery may be offered when the child is of primary school age. 5
The alveolus (gum) is the bony part of the upper gum through which teeth erupt. If the cleft involves the alveolus, this is repaired at the time of lip surgery. However, this can only be a soft tissue repair and the bony part of the alveolus will need to be joined together with a bone graft at around 8–12 years of age. Soft bone marrow is usually taken from the hip or the tibia and is put into the gum area to provide a stable base for the adult teeth to grow through. 5
Many children born with a cleft lip will be missing teeth, particularly around the area of the cleft. There is also the possibility of extra teeth, misshapen or poorly formed teeth. It is important that your child’s teeth are looked after carefully. From 18 months of age, it is important to have regular check-ups and care by a dentist experienced in the management of cleft. 6
Cleft palate
Clefts of the palate can vary in appearance and severity. The palate is made up of two main parts — a bony component called the hard palate and a muscular component called the soft palate. There can be a cleft of the soft palate alone, or a cleft can extend through both the soft and hard palate. 7
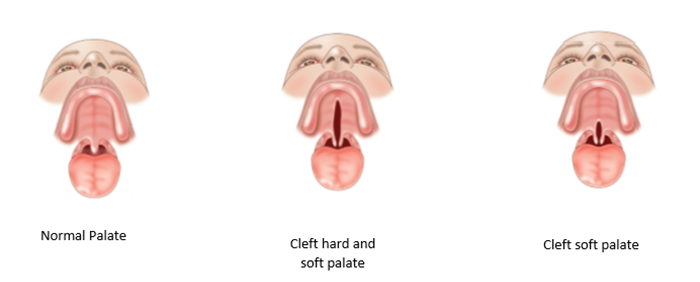
Figure 2. Types of cleft palate
Cleft lip and palate
The most common form of cleft involves the lip and palate and can affect just one side (unilateral cleft lip and palate) on the right or left, or both sides (bilateral). Each cleft varies in severity and extent, and care is best delivered within the multidisciplinary cleft team due to the complexity of care. Children with both a cleft lip and palate often require more frequent monitoring and therapy in the areas of speech, hearing and dentistry.
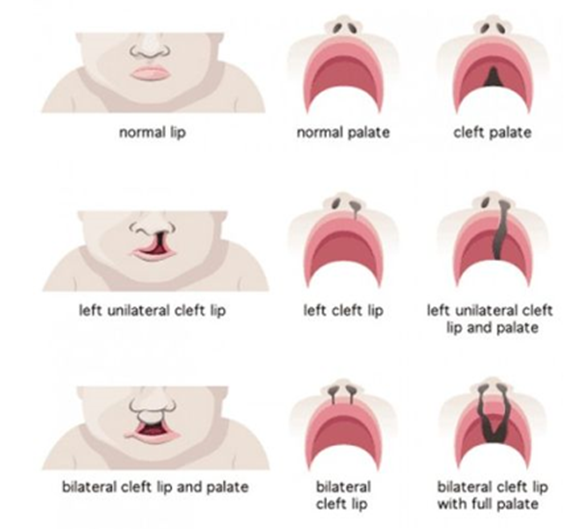
Figure 3. Different types of clefts
Submucous cleft palate
Usually the cleft in the palate is clearly visible. However sometimes the cleft is under the mucous membrane of the mouth — this is called a submucous cleft palate. 7
This type of cleft is often difficult to detect and may not be suspected unless an infant is having difficulties with feeding or until their speech begins to develop. A bifid (split) uvula is often the only sign of this type of cleft palate.
A small split in the uvula can occur without a cleft palate and may be present without any other problems. This is the most minor form of cleft palate, usually requiring no treatment.
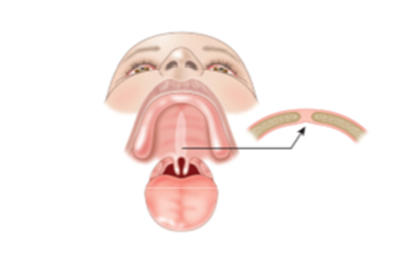
Figure 4. Submucous cleft palate
Pierre Robin Sequence
Pierre Robin sequence consists of three essential components 9, and can also be associated with cleft palate:
- micrognathia (small lower jaw or mandible)
- glossoptosis (posterior displacement of the tongue)
- airway obstruction.
The tongue is not actually larger than normal, but because of the small mandible, the tongue is displaced posteriorly thus obstructing the airway. Cleft palate can occur due to the posteriorly displaced tongue pushing on the palate during fetal development.
Immediately after birth, because of the small mandible and glossoptosis, many newborns have respiratory distress. These infants also have difficulty feeding and achieving adequate caloric intake.
Early management of cleft lip and palate
Depending on their needs, infants born with a cleft lip and / or cleft palate require care from a multidisciplinary cleft and craniofacial anomalies service, where an array of specialists from many fields are available. A referral to an outpatient cleft team is required at birth. Antenatal referrals can also be accepted.
Cleft and craniofacial teams
In Victoria there are two cleft and craniofacial teams:
Royal Children’s Hospital
Cleft Clinical Nurse Consultant
Phone: (03) 9345 6595
Fax: (03) 9345 6585
Email: plastic.surgery@rch.org.auMonash Children’s Hospital – Cleft & Craniofacial Anomalies Service
Referrals for Monash Children’s Hospital are accepted from registered Dental and Medical Practitioners and Consultants in relevant medical and surgical disciplines, and can be made via Monash Children’s Hospital
Specialist Consulting
Phone: (03) 8572 3004
Fax: (03) 8572 3007
Email: scmonashchildrens@monashhealth.org
Feeding a baby with a cleft lip/palate
Feeding patterns need to be established early to ensure good outcomes. 10 Some points to keep in mind:
- Babies born with a cleft lip alone usually breastfeed or bottle feed well.
- Babies with a cleft palate can’t create enough suction during feeding to draw milk from the breast or a regular bottle and require a specialised bottle and teat designed for babies with cleft palate.
Breastfeeding
Cleft lip only
- Babies born with a cleft lip alone usually breastfeed or bottle feed well.
- Some babies breastfeed better with the cleft facing upwards. The breast tissue usually fills the gap caused by the cleft and allows efficient feeding.
- Some bottle-fed babies feed better on a wide based teat.
- A referral to a lactation consultant and a speech pathologist should be made to provide support regarding positioning and maximizing feeding efficiency.
If you are concerned about a baby who has difficulty breathing or feeding due to airway obstruction, please refer to PIPER (1300 137 650).
Cleft lip and palate
- Babies with a cleft palate can’t create enough suction during feeding to draw milk from the breast or bottle easily. This is because air leaks from the nose to the mouth and the nose cannot be sealed from the mouth.
- If the infant has a cleft lip and a cleft palate, he/ she may not be able to compress the breast or teat well enough to push milk from the breast or bottle. In either case, feeding is usually slow and tiring and the baby may not drink enough to grow well.
- These problems are usually solved by using teats and bottles especially designed for babies with cleft palate. 11
Bottle feeding
A number of bottles are available: a SpecialNeeds® feeder; a Pigeon teat and a soft squeezy bottle; and a Chu Chu teat and a soft squeezy bottle. These bottles can be purchased from some pharmacies, the Equipment Distribution Centre (EDC) at The Royal Children’s Hospital, the Therapies Clinic at Monash Children’s Hospital or CleftPALS.
- Before feeding, practice squeezing the bottle and compressing the teat to be familiar with rate of flow and pressure required.
- Hold the baby in a semi-upright position to minimise the nasal regurgitation of milk.
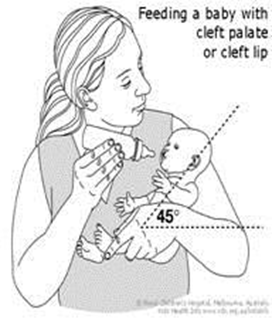
Figure 5. Feeding a baby with cleft palate or cleft lip
- Squeeze the bottle rhythmically only when the baby sucks (every two, three or five sucks). If you are using the SpecialNeeds® Feeder, the teat rather than the bottle should be squeezed. A squeeze every 3 – 4 sucks is usually sufficient however all babies are different so you may need to experiment a little with the rate of pulsing/squeezing.
- Have several breaks for burping, as the baby may be more windy than usual.
- Keep each feed to 20 – 30 minutes. Longer feeds mean the baby will use too much energy during feeding. This can lead to reduced weight gain. 10
- Watch a video demonstrating how to use the SpecialNeeds® feeder.
- Watch a video demonstrating how to use the Cleft Pigeon teat/bottle.

Figure 6. Feeders
Nasogastric tubes
In most cases a baby with a cleft lip and palate can be fully bottle fed. In some rare cases, when the baby is unable to feed successfully using a bottle, they may require a short-term nasogastric tube for feeding.
Surgery (plastic, ENT and oral surgery)
- Surgery is recommended at varying stages of development:
- lip repair between 3 and 6 months
- palate repair between 9 and 12 months
- insert ventilation tubes at time of palate repair
- more surgery when the child is older (5+ years ), if there is evidence of velopharyngeal insufficiency (VPI), for example, nasal speech
- bone graft to the cleft alveolus (gum) between 9 and 11 years in children who have a complete cleft of the lip and palate, if required
- adjustments of lip and nose shape when fully grown, if required.
Ongoing follow up
Audiology
Children with a cleft palate may have hearing problems due to a build-up of fluid in the middle ear. Children should have their hearing assessed at 4 weeks of age, and again at 12 weeks to determine if the hearing is compromised. These babies will often require insertion of middle ear ventilation tubes (grommets) at the time of palate surgery. 13
Dental, orthodontic and oral surgery
Children born with a cleft of the lip and/or palate are more at risk of dental decay. Therefore regular, good dental care is required from an early age.
Speech therapy
Most children who have a cleft palate repair will have speech which is normal or very close to normal. Some children may require speech therapy and/or further surgery. Routine speech reviews will be arranged every few years until growth is complete. 14
Consumer resources
- CleftPALS Vic
- Royal Children's Hospital Fact Sheets - cleft lip and palate infant feeding
- Australian Breastfeeding Association - Breastfeeding babies with clefts of lip and/or palate
- Royal Children's Hospital factsheets - cleft lip and palate
- CDC birth defects - cleft lip and palate
- Better Health Channel
References
- Mossey PA, Little J, Munger RG, Dixon MJ, Shaw WC. Cleft lip and palate. The Lancet. 2009 Nov 21;374(9703):1773-85. DOI:10.1016/S0140-6736(09)60695-4
- Victorian Congenital Anomalies Register. Congenital anomalies in Victoria 2015–2016, Melbourne: Consultative Council on Obstetric and Paediatric Mortality and Morbidity (CCOPMM), 2018. 48p.
- Wehby GL, Cassell CH. The impact of orofacial clefts on quality of life and healthcare use and costs. Oral diseases. 2010 Jan;16(1):3-10. DOI:10.1111/j.1601-0825.2009.01588.x
- Shi M, Wehby GL, Murray JC. Review on genetic variants and maternal smoking in the etiology of oral clefts and other birth defects. Birth Defects Research Part C: Embryo Today: Reviews. 2008 Mar;84(1):16-29. DOI:10.1002/bdrc.20117
- Royal Children’s Hospital Cleft Lip [pamphlet]. Melbourne VIC: Royal Children’s Hospital; 2015 [updated 2015 February; cited 2019 August].
- Haque S, Alam MK. Common dental anomalies in cleft lip and palate patients. The Malaysian journal of medical sciences: MJMS. 2015 Mar;22(2):55.
- Royal Children’s Hospital Cleft palate [pamphlet]. Melbourne VIC: Royal Children’s Hospital; 2015 [updated 2015 February; cited 2019 August].
- Cleft Connect Australia. Different types of cleft [Image on internet]. 2018 [cited August 2019]. Available from: http://cleftconnect.org.au/everything-about-cleft
- Randall P, Krogman WM, Jahina S. Pierre Robin and the syndrome that bears his name. The Cleft palate journal. 1965 Jun 30;2(3):237-46.
- Reilly S, Reid J, Skeat J, Cahir P, Mei C, Bunik, and the Academy of Breastfeeding Medicine M. ABM Clinical Protocol# 17: Guidelines for breastfeeding infants with cleft lip, cleft palate, or cleft lip and palate, Revised 2013. Breastfeeding Medicine. 2013 Aug 1;8(4):349-53. DOI:10.1089/bfm.2013.9988
- The Royal Children’s Hospital Melbourne. Cleft lip and palate – infant feeding [pamphlet]. Melbourne VIC: Royal Children’s Hospital; 2015 [updated 2015 February; cited 2019 August].
- The Royal Children’s Hospital Melbourne. Cleft lip and palate – infant feeding [Internet]. Melbourne VIC: Royal Children’s Hospital; 2018 [updated 2018 June; cited 2019 August].
- The Royal Children’s Hospital Melbourne. Cleft and hearing [pamphlet]. Melbourne VIC: Royal Children’s Hospital; 2015 [updated 2015 February; cited 2019 August].
- The Royal Children’s Hospital Melbourne. Cleft palate and speech [pamphlet]. Melbourne VIC: Royal Children’s Hospital; 2015 [updated 2015 February; cited 2019 August].
Citation
To cite this document use: Safer Care Victoria. Cleft lip and palate [Internet]. Victoria: Neonatal eHandbook; 2024 [cited xxxx] Available from: https://www.safercare.vic.gov.au/clinical-guidance/neonatal
Download this guidance
Get in touch
Version history
First published: July 2015
Reviewed: October 2024