Please note that some guidelines may be past their review date. The review process is currently paused. It is recommended that you also refer to more contemporaneous evidence.
If unfamiliar with the technique of intubation, continue to provide mask ventilation until experienced help arrives. Most infants can be adequately managed with effective positive pressure ventilation (PPV) using a T-piece device or a self-inflating bag and mask.
In an emergency, oral intubation is recommended. Nasal intubation may be considered if longer term ventilation is anticipated. The route chosen will also depend on the training and skill of the operator. Intubation without premedication is warranted in severely compromised infants at birth, or in life threatening situations.
In less urgent situations, premedication should be considered. This may include use of a short acting muscle relaxant. Muscle relaxants are contraindicated in situations known to be associated with difficult intubation (for example, Pierre Robin sequence, and other airway anomalies) or when the operator is inexperienced with intubation or with these medications.
Indications
Common indications for intubation include:
- neonatal resuscitation where PPV using a T-piece device/self-inflating bag and mask ventilation is ineffective or prolonged, evidenced by bradycardia (HR<100 bpm), falling oxygen saturations or failure to reach target oxygen saturation ranges
- special circumstances, such as congenital diaphragmatic hernia, extreme prematurity
- frequent apnoea requiring intervention
Infants born without a detectable heartbeat should be intubated as quickly as possible during resuscitation at birth.
Equipment
Equipment required for neonatal intubation (Figure 1):
- laryngoscope handle
- blades: 00, 0 (premature), 1 (neonatal)
- introducer (stylet) for oral intubation only - inserted to 1 cm less than the length of the ET tube. This is optional - not all operators use an introducer (stylet)
- Magills forceps for use during nasal intubation only
- endotracheal tubes: appropriately sized uncuffed ET tubes: 2.5mm, 3.0mm and 3.5 mm (see Table 1) weight
- tapes for securing ET tubes – gauze to remove vernix from face (if needed), hydrocolloid dressing to protect the skin (e.g. DuoDERM® Comfeel), and Leukoplast or similar for securing the ETT.
- colorimetric end-tidal CO2 detector (PediCap™ or similar) (Figure 2)
- syringes and needles for premedication (see Premedication)

Figure 2: PediCap TM colorimetric end tidal CO2 detector
Other equipment required for intubation:
- T-piece device (or self-inflating bag (240 mL)) with appropriately sized face mask
- Medical gases, air and oxygen with flow meter and tubing allowing flow rate up to 10 L/min with oxygen/air blender
- Suction apparatus and suction catheters (6Fg or 8Fg and 10Fg or 12Fg)
- stethoscope (Neonatal size preferable)
- Monitoring (cardio-respiratory and pulse oximetry)
- Feeding tube for gastric decompression (8Fg or 10Fg) and 10mL syringe
Endotracheal tube (ETT) size
The choice of ETT internal diameter (ID) can be estimated as gestational age in weeks divided by 10. Using this rule, a 2.5mm ID endotracheal tube would be used for an infant born at 25 weeks’ gestation, a 3.0mm ID for an infant born at 30 weeks and a 3.5mm ID for an infant born at 35 weeks’ gestation.
A more accurate means of assessing the appropriate size tube is using a combination of gestational age (GA) and weight, as recommended by the Australian Resuscitation Council (2016).
Table 1 provides a guide to ETT size and depth of insertion (to the nearest 0.5cm), measured at the lip (oral intubation) or the ala of the nostril (nasal intubation) using the gestational age and weight guideline.
Table 1: ETT tube size and length by corrected gestation and weight
|
Corrected gestation |
Weight |
ETT size |
Depth of insertion at the lip (cm) |
Depth of insertion at the nare (cm) |
|---|---|---|---|---|
|
23 - 24 |
0.5 - 0.6 |
2.5mm
|
5.5 |
6.5 |
|
25 - 26 |
0.7 - 0.8 |
6.0 |
7.0 |
|
|
27 - 29 |
0.9 - 1.0 |
6.5 |
7.5 |
|
|
30 - 32 |
1.1 - 1.4 |
3.0mm |
7.0 |
8.0 |
|
33 - 34 |
1.5 - 1.8 |
7.5 |
8.5 |
|
|
35 - 37 |
1.9 - 2.4 |
3.5mm
|
8.0 |
9.0 |
|
38 - 40 |
2.5 - 3.1 |
8.5 |
9.5 |
|
|
41 - 43 |
3.2 - 4.2 |
9.0 |
10.0 |
An alternative method of estimating the depth of ETT insertion is using the 'rule of six'.
Oral ETT depth at lips (cm) = Weight [kg] + 6cm
Nasal ETT depth at nares (cm) = (Weight [kg] x 1.5) + 6cm
N.B. The 'rule of six' calculation may overestimate depth of ETT position for an oral tube (ETT inserted too far), and underestimate depth of ETT for a nasal tube (ETT not in deep enough). These calculations are especially inaccurate in infants <750g, resulting in over-estimation of ETT insertion depth.
The gold standard of confirming correct placement of the endotracheal tube is by chest X-ray. Clinical signs of correct placement in the trachea should be assessed immediately post intubation (see Procedure).
Monitoring
Pulse oximetry is recommended to monitor heart rate and to assess oxygen saturation (SpO2). Cardio-respiratory monitoring is highly desirable but may not be immediately available during an acute cardiorespiratory arrest or in the delivery room. If available, it should be used.
Prior to an elective or controlled intubation, place the infant under a radiant warmer, establish intravenous (IV) access, attach cardiorespiratory and pulse oximetry monitoring and record a full set of baseline observations. Allocate medical and nursing team roles e.g. medication administration, suction, intubation, securing of the ETT, scribe.
Anticipate the need/pathway for escalation in the management of a difficult airway.
Anticipate the need for a chest x-ray and a radiographer (especially if not onsite at the hospital).
Premedication
Premedication is recommended except in emergency intubation during resuscitation. Premedication reduces pain, discomfort, traumatic injury to the airway and physiologic instability associated with intubation/ laryngoscopy.
Physiological responses to intubation may be reduced/eliminated by using:
- Vagolytic – atropine
- Rapidly-acting analgesia – fentanyl
- Short-duration muscle relaxant - suxamethonium
As neuromuscular paralysis develops, commence positive pressure ventilation with a T-piece (or self-inflating bag) and then intubate. Use of muscle relaxants is contraindicated if there are concerns about being able to maintain the airway should intubation be unsuccessful.
Atropine should be available and may be used prior to suxamethonium for intubation to avoid bradycardia. Do not give in the presence of significant hyperkalaemia (serum K+ > 7mmol/L in non-haemolysed arterial or venous blood).
Neonates are more sensitive to neuromuscular blocking agents compared with adults. Suxamethonium may cause reactive bradycardia and increased salivation; however, this is uncommon with single doses.
Premedication drugs and doses are outlined in the table below.
Medicine |
Atropine |
Fentanyl |
Suxamethonium |
|---|---|---|---|
|
Concentration |
600 mcg/mL |
100 mcg /2 mL |
100 mg /2 mL |
|
Route |
IV |
IV |
IV |
|
Dose |
20 mcg/kg |
5 mcg/kg |
2 mg/kg |
|
Weight (g) |
|
|
|
|
500 |
0.02 mL |
0.05 mL |
0.02 mL |
|
750 |
0.03 mL |
0.08 mL |
0.03 mL |
|
1,000 |
0.03 mL |
0.1 mL |
0.04 mL |
|
1,250 |
0.04 mL |
0.13 mL |
0.05 mL |
|
1,500 |
0.05 mL |
0.15 mL |
0.06 mL |
|
1,750 |
0.06 mL |
0.18 mL |
0.07 mL |
|
2,000 |
0.07 mL |
0.2 mL |
0.08 mL |
|
2,500 |
0.08 mL |
0.25 mL |
0.1 mL |
|
3,000 |
0.1 mL |
0.3 mL |
0.12 mL |
|
3,500 |
0.12 mL |
0.35 mL |
0.14 mL |
|
4,000 |
0.13 mL |
0.4 mL |
0.16 mL |
|
4,500 |
0.15 mL |
0.45 mL |
0.18 mL |
|
5,000 |
0.17 mL |
0.5 mL |
0.2 mL |
Intubation medications should be administered in the following order:
- Atropine (over 60 seconds and flush, wait for a rise in HR of >20 bpm).
- Fentanyl (slowly over 30 seconds, and then flush slowly). If morphine is used instead of fentanyl, administer as a bolus dose of 100 mcg/kg/dose
- Suxamethonium (over 10-30 seconds).
If intubation is unsuccessful, suxamethonium can be administered again, but atropine and fentanyl (or morphine) should not be repeated.
Procedure
- Observe standard precautions.
- Maintain sterility of equipment until use. Use a new endotracheal tube for each intubation attempt. Do not leave the ETT under a radiant heat source - this makes the ETT soft and difficult to insert.
- Aspirate stomach contents prior to procedure if the infant has been fed recently.
- Position the infant’s head in the slightly extended ‘sniffing’ position. Do not hyper-extend the head - this impedes visualisation of the airway.
- Holding the laryngoscope in the left hand, gently open the mouth and insert the laryngoscope.
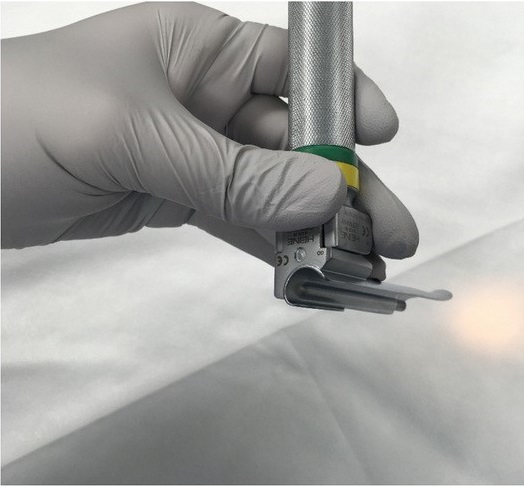 Figure 3a
Figure 3a
Pass the laryngoscope blade gently along the right side of the open mouth and over the tongue until the epiglottis comes into view.
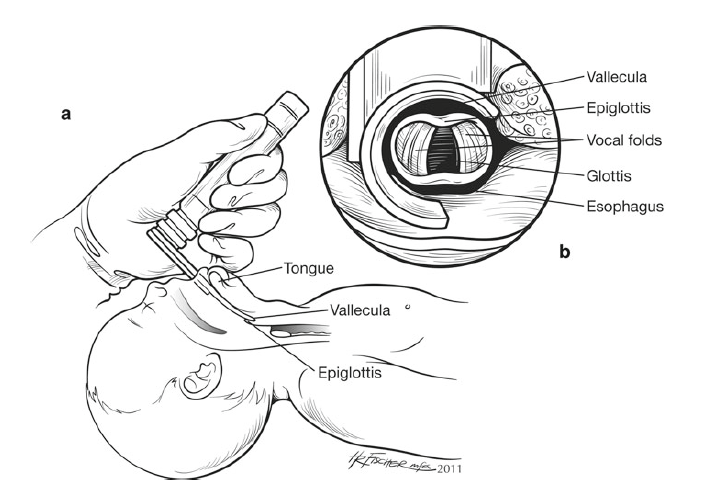 Figure 3b
Figure 3b
Continue to advance the blade until the tip sits in the vallecular. Gently lift the blade forwards and upwards until the vocal cords come into view.
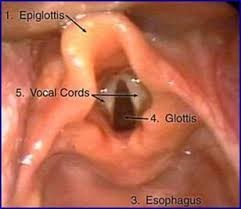 Figure 3c
Figure 3c
Figure 3: Correct technique for a) holding the laryngoscope, b) inserting the blade and c) visualising the vocal cords and surrounding anatomical landmarks
(N.B. Avoid ‘rocking’ backwards - this can injure the gums and potentially future dentition.)
If the vocal cords and epiglottis do not come into view, withdraw the laryngoscope back gradually until the cords are visualised (Figure 3c). This is important in avoiding accidental intubation of the oesophagus. Application of cricoid pressure may be helpful to bring the larynx into view. Suction any secretions obstructing the view of the airway.
Holding the ETT between the index finger and thumb, insert the ETT at a 90° angle from the right side of the mouth, insert the ETT 1-2 cm through the vocal cords using the vocal cord marker as a guide. Holding the ETT against the palate of the mouth with the right hand, carefully remove the laryngoscope blade and the stylet /introducer (if used), taking care not to dislodge the ETT.
6. If the infant is bradycardic for > 30 seconds during the procedure and intubation is not near complete, remove the ETT tube and provide positive pressure ventilation with a mask until the heart rate and oxygen saturation (SpO2) return to baseline/normal limits, before attempting intubation again.
7. If there is no improvement in heart rate and SpO2 post intubation, and/or no change in colour of the end tidal CO2 detector, be aware that intubation of the oesophagus or right main bronchus may have occurred. If this is suspected, remove the ETT and stabilise the infant using positive pressure ventilation before another attempt.
8. Following insertion of the ETT, confirm that the tube is in the correct position. The tip of the ETT tube should lie approximately midway between the vocal cords and the carina, at thoracic vertebrae T2-T3, this can only be verified on chest x-ray. Until an x-ray can be obtained, the following clinical signs should be assessed to determine if the tube is in the trachea.
Clinical signs of tracheal intubation include:
- Visualising the endotracheal tube pass through the vocal cords (at the black 'vocal cord' marker on the tube)
- An increase in the infant’s heart rate >100 bpm with positive pressure ventilation via the ETT
- Equal breath sounds heard in both axillae with a stethoscope (this can be difficult in extremely preterm infants as sound is heard throughout the chest)
- Listen over the stomach - air entry heard over the stomach, especially if louder than over the axillae, may indicate oesophageal intubation
- Symmetrical chest movement seen with each positive pressure inflation
- Positive result on end-tidal CO2 detector on exhalation
- Vapour (misting) seen in the ETT on exhalation
- Improvement in colour and oxygen saturation
(N.B. May not be evident in an infant with congenital heart disease or severe pulmonary hypertension)
9. Securing the ETT
The person in charge of the airway should hold the ETT in position until it is secured, ensuring the tube does not dislodge while it is being taped. Figure 4 illustrates one method of securing an oral ETT.
| Figure 4a: Cut two Leucoplast® tapes as shown. The length of the cut out thin section should be approximately twice the width of the infant’s mouth. The end sections should be no longer than the distance between the edge of the infant’s mouth and the infant’s ear |
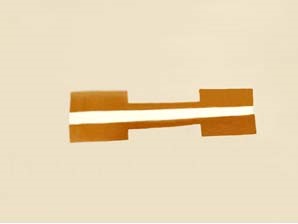 Figure 4a
Figure 4a
|
|
Figure 4b: Dry the face and apply hydrocolloid dressing to protect the skin on either side of the cheeks. Optional: Use a length of cotton tie to secure the ETT, ensuring the tie is long enough so the string ends can be captured by the tapes for additional stability. |
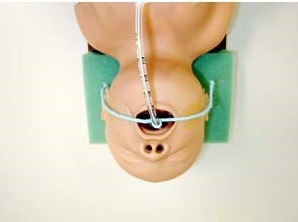 Figure 4b
Figure 4b
|
|
Figure 4c: Start applying the first tape by placing the edge of the wide section as closely as possible to the corner of the mouth. If used, ensure the tie is pulled firmly and captured by the tape. Wind the tape several times around the ETT before securing on opposite side. |
 Figure 4c
Figure 4c
|
|
Figure 4d: Completion of the first tape |
 Figure 4d
Figure 4d
|
|
Figure 4e: Next, apply the second tape. Repeat the same process as for the first tape, but start from the opposite side. |
 Figure 4e
Figure 4e
|
|
Figure 4f: The ETT is now secured. |
 Figure 4f
Figure 4f
|
Alternative method of securing oral ET tube ('Trouser legs')
- Dry the face and apply hydrocolloid dressing strips on the upper lip and cheeks, protecting the skin where the securing tapes will be placed.
- Adhere the unsplit section of one 'trouser' to the cheek and one tab on or above the upper lip. Wrap the other tab in a spiral around the ET tube.
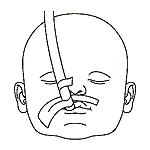 Figure 5, step 1
Figure 5, step 1
3. Take the second 'trouser' and adhere the unsplit section to the cheek. Place one tab below the lower lip and wrap the other tab in a spiral around the ET tube
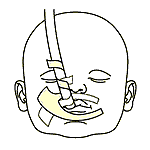 Figure 5, step 2
Figure 5, step 2
Laryngeal mask airway (LMA)
Use of an laryngeal mask airway (LMA) has not been fully evaluated in newborns or established yet as standard practice in neonates (although they are used routinely in short surgical procedures as an alternative to intubation). Unlike an ETT, an LMA cannot be used for drug administration (adrenaline, surfactant)
A LMA has been designed to enable assisted ventilation without passage of an ETT tube through the vocal cords and may be considered in infants >34 weeks’ gestation and/or >2000g if:
- Mask ventilation is not successful
- Tracheal intubation is unsuccessful or not feasible
A size 1 LMA is appropriate for infants >34 weeks’ gestation and/or >2000 weight. This is the smallest size LMA currently available.
More information
Clinical guidelines and consensus statements
Australian and New Zealand Committee on Resuscitation (2016). Guideline 13.4: Tracheal Intubation and ventilation of the newborn infant
The Victorian Newborn Resuscitation Project, NeoResus (2017). Endotracheal intubation
Royal Children’s Hospital. Clinical Guidelines (Nursing). (2017). Assisting with elective intubation of the neonate on the Butterfly ward
References
Australian and New Zealand Committee on Resuscitation 92016). Guideline 13.4: Tracheal intubation and ventilation of the newborn infant
Schmölzer, G.M; O'Reilly, M., Davis P.G, Cheung P.Y & Roehr C. C. (2013). Confirmation of correct tracheal tube placement in newborn infants. Resuscitation, 84 6): 731-737. DOI 10.1016/j.resuscitation.2012.11.028
Spence, K and Barr, P. (2000). Nasal versus oral intubation for mechanical ventilation of newborn infants. Cochrane Database of Systematic Reviews. (2): CD000948. DOI 10.1002/14651858.CD000948
Grein, A.J., & Weiner, G.M. (2005). Laryngeal mask airway versus bag and mask ventilation or endotracheal intubation for neonatal resuscitation (review). Cochrane Database of Systematic Reviews, (2): CD003314. DOI 10.1002/14651858.CD003314.pub2
Kamlin, C.O; O’Connell, L.A; Morley, C.J; Dawson, J.A; Donath, S.M; O'Donnell, C.P; & Davis P.G. (2013). A randomized trial of stylets for intubating newborn infants. Pediatrics, 131 (1): e198-205/ DOI 10.1542/peds.2012-0802.
Kumar, P., Denson, S.E., Mancuso, T.J., Committee on Fetus and Newborn, Section on Anesthesiology and Pain Medicine (2010). Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics, 125(3): 608-615. DOI: 10.1542/peds.2009-2863.
Get in touch
Version history
First published: August 2015
Review by: August 2018

