Transcript
View more View lessSafer Care Victoria
Improving Sexual Safety – Mental Health Inpatient Units
Video Transcript – August 2025
Prepared for internal and external distribution.
Transcript – Improving Sexual Safety - Mental Health Inpatient Units
GRAPHICS:
Safer Care Victoria logo
Improving Sexual Safety
Mental Health Inpatient Units
Mental Health Improvement Program logo
00:00:10 – Misha Adair
Improving sexual safety in mental health services is a first-of-its-kind initiative – part of Safer Care Victoria’s Mental Health Improvement Program.
00:00:19 – Misha Adair
The 2021 Royal Commission into Victoria’s Mental Health System recommended this important work be done to drive changes and improvements that help create safety for all.
00:00:30 – Misha Adair
We’re working with inpatient units to trial and implement real solutions that positively impact the experience of sexual safety for consumers, carers, and staff, and reduce sexual safety incidents.
00:00:49 – Misha Adair
This is breaking new ground. There’s no established foundation of evidence for these improvements. We’re building it here in Victoria, with services leading the way globally.
GRAPHICS:
Peninsula Health, Frankston
00:00:59 – Alysha Bonell
One of the biggest shifts we made was understanding that safety isn’t just about what staff do. It’s about mutual responsibility. Consumers have a right to feel safe, and they also play a role in making others feel safe too.
00:01:12 – Alysha Bonell
Our first step was defining sexual safety in a way that made sense to everyone – consumers, carers, and the staff.
00:01:19 – Courtney Dunn
We co-designed sexual safety plans with our consumers, lived experience workforce, and clinicians to ensure it wasn’t just another policy, but something meaningful.
00:01:27 – Courtney Dunn
It was important to recognise that it’s new to everyone, consumers and staff alike, and we’re all learning together
00:01:34 – Alysha Bonell
Now these plans are becoming part of our admission process. The moment someone arrives, we want them to know: your sexual safety matters here, and we will work with you so you feel safe within our service.
GRAPHICS:
Eastern Health, Ringwood
00:01:47 – Laura Rizert
One of our biggest challenges was helping staff feel comfortable and confident in discussing sexual safety. Some weren’t sure how to respond to disclosures or felt uncomfortable talking about it, whilst others didn’t always recognise certain behaviours as harassment.
00:02:06 – Laura Rizert
We promoted a greater awareness of sexual safety and introduced staff education sessions to change that. Now we see more open conversations and staff advocating for both consumers and themselves with confidence.
00:02:14 – Brittany Williams
We also introduced a sexual safety wall – a simple but powerful tool that provides clear information on healthy boundaries, STI screening, and support services like ECASA. It’s a daily reminder that sexual safety is a priority and not an afterthought.
00:02:29 – Brittany Williams
With our simple tracking board, we ensure all consumers receive and understand their bedroom access wristbands.
00:02:35 – Laura Rizert
Before, they relied on staff with keys. Now they have control over their own space. It’s made a huge difference in how safe and in control consumers feel.
00:02:47 – Alysha Bonell
When we first started testing these interventions, we recognised that even though staff had been having these discussions with consumers informally, we needed to better support the quality of the practice and to make it more consistent across the multidisciplinary teams.
00:03:00 – Alysha Bonell
But once we started having these discussions at a deeper level, something changed.
00:03:05 – Courtney Dunn
Consumers shared experiences they hadn’t felt significant enough to report before. Just by making it more visible, people were more aware that sexual safety was just as critical as other safety measures on the ward.
00:03:17 – Alysha Bonell
That was the turning point. It showed us why this work matters and why we need to commit to continuous improvement. That we needed to pause, reevaluate, and readjust as we move forward to embedding sexual safety practices in our service.
00:03:33 – Misha Adair
The mental health inpatient teams we’re working with are forging the way for understanding practical approaches to improving sexual safety for all.
00:03:42 – Misha Adair
They’ve challenged assumptions and listened to a variety of perspectives to thoughtfully consider, trial, and examine improvements that place the consumer at the heart. This work will make real, positive difference in how everyone experiences safety.
GRAPHICS:
Mental Health Improvement Program
Safer Care Victoria logo
About the initiative
The first of its type, this initiative supports participating services to trial a range of targeted changes aimed at improving sexual safety in inpatient units for consumers, their carers, families and supporters and workforce.
Improving sexual safety within mental health inpatient units includes reducing instances of:
- sexual assault
- sexual harassment
- other sexual incidents
The initiative aims to see participating services:
- reduce the rate of sexual safety incidents by 20 per cent (per 1,000 bed days)
- increase self-reported experiences of sexual safety by 20 per cent for consumers, their families and carers and the workforce.
How we support services
The MHIP supports participating mental health inpatient services to design and test changes:
- with crucial input from Lived and Living Experience workforce members
- within their existing resources and infrastructure to support sustainable change that fits with their unique context
- to help improve the quality and experience of care and create a safer experience for all Victorians in mental health inpatient units
Examples of these changes include:
- improving communication on reporting tools if someone feels unsafe
- expanding and adding risk assessments and safety plans.
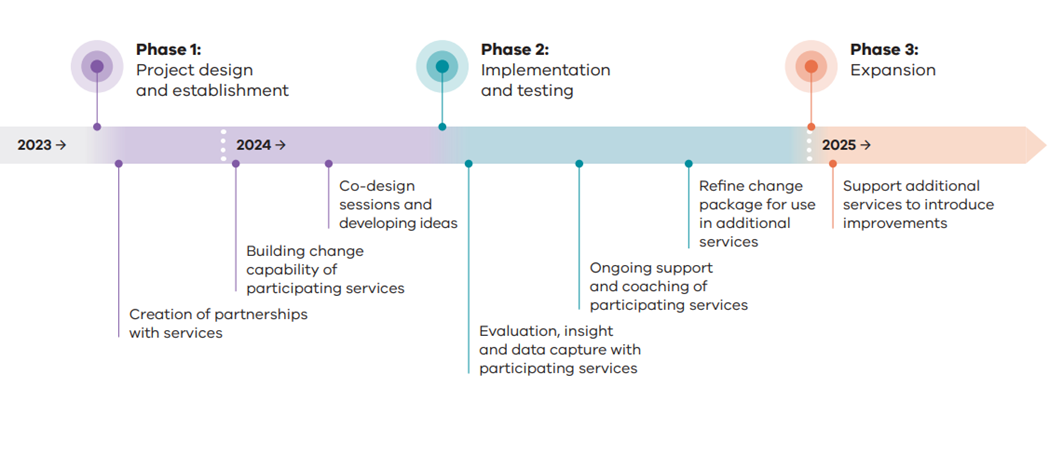
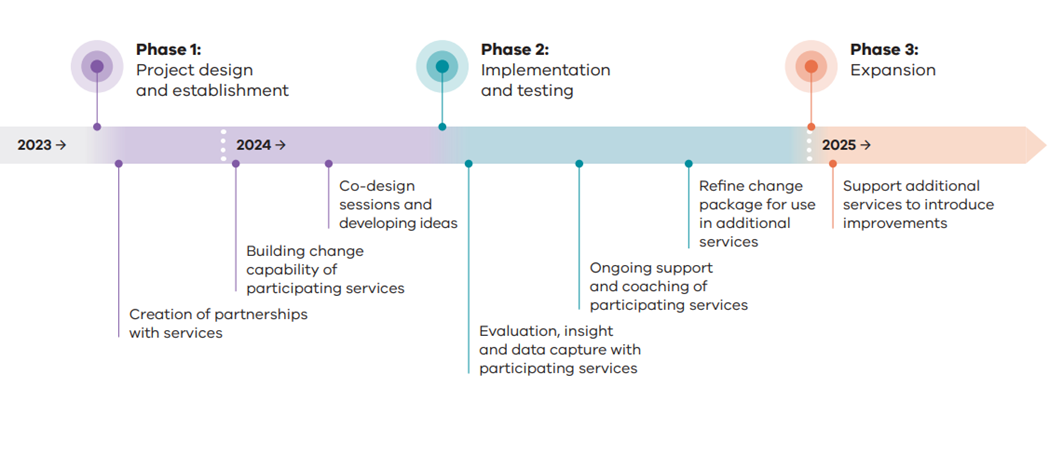
Path ahead
Together, the MHIP and participating services are continuing to collect, review and analyse data throughout the implementation and testing phases. The findings and insight will inform how additional mental health and wellbeing services can be supported to introduce improvements to their respective inpatient units from 2025.