On this page
About the toolkit
Our Quality Improvement Toolkit includes fact sheets, practical tools, templates and resources to help you improve the quality of care in Victoria.
These tools help you to:
- gain a better understanding of problems
- identify solutions
- develop and measure effective improvement strategies and activities.
Download the toolkit
Individual fact sheets and templates
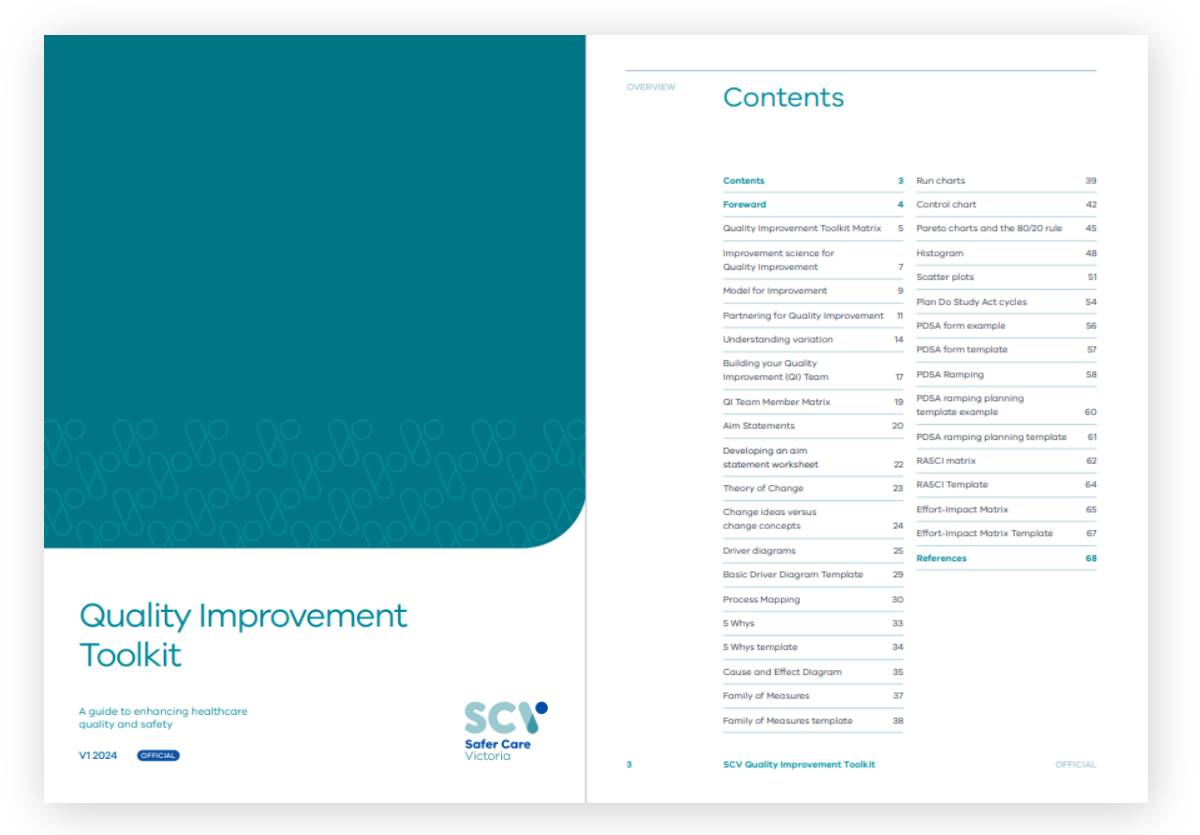
This toolkit includes individual fact sheets, tools, and templates, available to download below.
Templates
- Cause & effect template (Tool 12)
- Run Chart template (Tool 14)
- Pareto Chart template (Tool 16)
- Histogram template (Tool 17)
- Scatter Plot template (Tool 18)
- PDSA long form template (Tool 19)
- PDSA short form template (Tool 19).
Download fact sheets and templates
More resources
- Victorian Clinical Governance Framework
- Partnering in healthcare framework
- Department of Health Cultural Responsiveness framework – Guidelines for Victorian health services
- Department of Health Designing for Diversity framework
- IHI Achieving Health Equity - A Guide for Health Care Organisations
- IHI Psychology of change framework
- IHI Toolkit
- CEC Toolkit
Feedback
If you have any feedback, or are seeking additional information or please email culture.capability@safercare.vic.gov.au.